
In our new monthly report, FPM looks in detail at what the CQC have reported from their GP practice inspections during November 2025. Using publicly available reports on the CQC website, we highlight some of the behaviours that won practices Outstanding ratings, and the reasons some practices were scored Requires Improvement, or Inadequate. Do you recognise any of the observations the CQC picked up, either good or bad? Do you think the CQC's findings are fair?
Going forward, these reports will only be sent out in our refreshed FPM Group newsletter - sign up here to be on the mailing list!
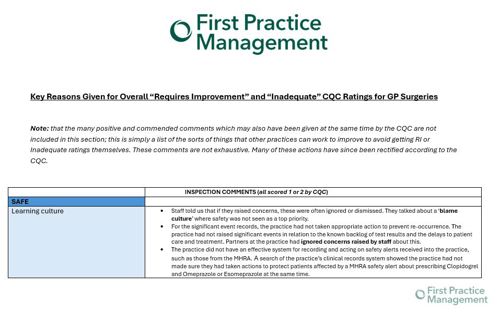
In the inspection reports published during Nov 2025, the following common themes emerged (for full report click the image or the link below).
Policies and Compliance
- Policies being created but not embedded: “A clinical supervision policy had been created in June 2024 however; we did not see evidence that this had been embedded yet. “
- Policies being created which are not specific to the practice: “There was an Access Control policy in place, but this was not specific to the practice.”
- Policies not being followed: “Although the practice had implemented a new system for complaints, patients did not always receive a written outcome, which was not in line with the practice policy.” “The practice had a recently implemented performance appraisal policy and procedure; however, we found that this was not being adhered to. We did not see any annual formal appraisals in staff files.”
- Policies in place but no associated protocol: “We noted that the practice’s cold chain policy detailed that daily temperature checks should take place in addition to the use of a data logger and the practice should consider implementing a protocol to ensure that staff were available to deputise in the absence of staff who normally conducted the temperature checks.”
Our market leading compliance software FPM Core lets you know who has read what policies, and when, so you are always up to date with compliance - click here to book your demo today
Gaps in Training
- Patient notes summarising is sometimes delayed and leads to poor ratings: “At the time of the inspection, there was a backlog of 120 new patient records awaiting summarisation”
- Medicines optimisation remains worst scoring category for practices: some practices were rated good or outstanding for the entire Safe category, apart from Medicines Optimisation, for which they scored 1 – meaning their overall Safe category score was downgraded to Requires Improvement.
- Basic training not being adhered to: “training records we reviewed did not demonstrate that all staff were up to date with basic life support and sepsis awareness training.” “We did not see evidence that staff had consistently completed or had undertaken training in basic life support, fire safety, Mental Capacity Act, safeguarding adults and children (to the appropriate level for their role) and sepsis awareness training.”
Thornfields expert healthcare training can train you and your staff to give them the skills they need. Click to browse our workshops for individuals and organisations.
Issues with Websites
- Websites not being kept up to date: “the practice’s website was not always kept updated to keep people well informed.”
- Websites not being easy to use or contact the practice on: “28% of patients who responded found it easy to contact the practice using their website. This was lower than the local average GP score of 46% and the national average score of 48%”.
Click here to learn about the market-leading websites that My Surgery Website can create for you.
Examples of Outstanding Care
- Caring: focusing on the identification of young carers and were utilising their close working relationship with a local high school and college - a care co-ordinator had met with the deputy head teacher, and a GP had done a talk at a local college on careers in medicine with the students; use of wellbeing noticeboard which showcased what the team had been doing in their spare time; a picnic bench in the gardens for staff; anonymous feedback via a QR code displayed in the staff areas.
-
Responsive: a practice had identified the 4% of patients who used 20% of appointments, put a flag on their record and offered them longer, holistic review appointments; use of fully computerised pathology lab system and staff utilised ‘Healthshare’ software to access hospital data; use of a four-week rota so GPs could book their own follow up appointments before a patient appointment finishes; 3 members of staff who were NHS App ambassadors that champion the NHS App and provide guidance and support for patients; practice had established an excellent rapport with local farms who employed mainly overseas workers seasonally.
-
Well-led: staff rewarded through Going the Extra Mile scheme and created a recognition of long service and team achievements; all staff members were involved in shaping the new vision and values through Protected Learning Time (PLT) workshops; a practice had established a Carers Network following direct feedback from patients registered as carers at the practice. The first event took place in September 2025 and over 40 carers and 5 external support organisations, alongside key practice staff and the Carers Champion attended.


0 Comments