
In this monthly report, FPM looks in detail at what the CQC have publicly reported from their GP practice inspections during December 2025. Only the most notable/useful comments are selected for readers from amongst thousands. We highlight some of the behaviours that won practices Outstanding ratings, and the reasons some practices were scored Requires Improvement, or Inadequate. Do you recognise any of the observations the CQC picked up, either good or bad?
Outstanding (scores of 4):
There were some truly outstanding and creative behaviours in some of the "outstanding" reports:
-
Patient passports: "Patients with learning disability were asked to attend their annual review during their birthday month. The practice created a passport where the patient could add things that were important to them, and this could be worn as a lanyard. For example, patients could highlight ‘things to know and ways to help me: give me specific instructions and explain why, check my understanding, ask me direct (closed) questions’."
-
Walking groups: "The practice had created a Walking Group, and a pilot for patients suffering with chronic pain using a more holistic approach. Following training one of the GPs invited 20 patients to attend 4 sessions held at a Community Garden"
-
Free seminars in local church: "The practice organised annual free seminars for patients and residents at a local church. Past topics included generalised anxiety, women’s health and challenges associated with ageing."
-
Gifts and winter coats: Staff within the practice told us that they provide gifts to patients in care homes who have no family at Christmas time. Staff had run an initiative to ensure all children in the local community had access to a winter coat.
- "Healthcare" not "surgery": Management told us when they chose the name of the practice, they had made a conscious decision to call it “[location] Healthcare” and not “surgery” or “practice” as they did not want the practice to be medically led but have a holistic approach to healthcare.
Click on the image below to read the full report
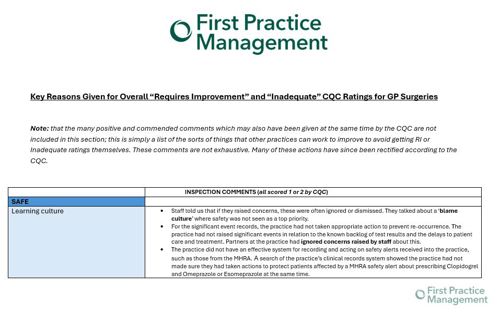
Requires Improvement / Inadequate (Scores of 1 or 2):
-
Practices didn't reflect policies: "Operational practices were not accurately reflected in the provider’s policies - different forms were being used than those stated and designed to support staff and promote effective and defensible decision making; The practice had a staff immunisation policy. However, we found that this was not always being followed, and the practice had not evidenced staff immunisations in line with UK Health Security Agency Guidance." "There was an Access Control policy in place, but this was not specific to the practice".
Our market leading compliance software FPM Core lets you know who has read what policies, and when, so you are always up to date with compliance - click here to book your demo today
-
Complaints not handled correctly: Complaints were stored within patient clinical records, which could leave the patient open to future prejudice.
-
No process in place for violent behaviour: "Staff reported episodes of aggression from the public including racially motivated abuse. The practice did not have a clear process in place to manage these incidents and found it hard to identify how they could prevent further episodes."
-
Poor coding: "there was no established and effective system in place to ensure consistent and accurate coding of clinical information; another practice had not completed any formal audits of the summarising process."
-
Risk assessments not updated: "when the practice made changes, risk assessments were not always updated accordingly, e.g. after relocating the oxygen storage from one room to another, the hazard signage was not updated to reflect the new location."
-
DBS checks policy not followed: "checks were not always carried out in line with the practice policy and where DBS checks had not been completed there were not documented risk assessments. Lack of processes in place to confirm whether appropriate recruitment checks, or training had been undertaken by clinical staff employed by the PCN but who were working under the direction of the practice."
-
Multiple gaps in training: "we found gaps in up-to-date training for safeguarding children, safeguarding adults, preventing radicalisation, mental capacity act, infection prevention and control, fire awareness, sepsis and equality and diversity."
Thornfields expert healthcare training can train you and your staff to give them the skills they need. Click to browse our workshops for individuals and organisations.
-
Significant events not managed - reports lacking detail relevant to investigating the incident and documented action.


0 Comments